T1D at School: putting the support plan into action
Michelle MacPhee
D-Mom, M.S. (Psychology)
So you have written a fantastic, concise, comprehensive Care Plan for your T1D child at school… now what?
The next step is to figure out how to put that plan into action by sitting down with your key contact(s) at your child’s school (this may be a teacher, the principal, the school nurse, a teaching assistant, or a combination of these people). At this meeting you could discuss: Who will do what and when? Where will supplies be stored, where will your child check her blood glucose? What structures and procedures need to be created at school to keep your child safe and available for learning? What do you need to do from home to keep things running as they should?
(For more on who does what, check out Roles & Responsibilities for School Care)
Planning the Day
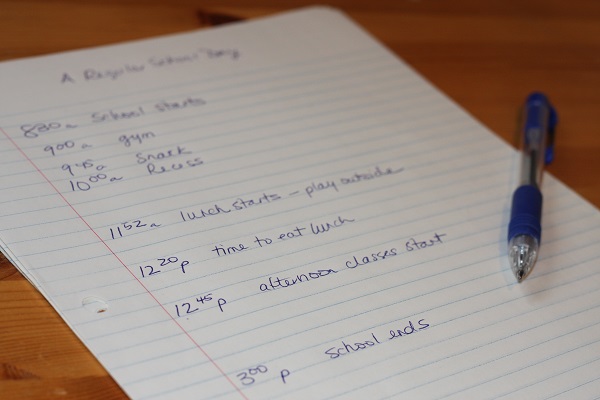
A good place to start is with the existing school schedule. School staff can tell you what a typical day may look like, including when recess, lunch and physical education classes occur, as well as any other day-to-day events that may affect your child’s blood glucose. At our school meeting, I jotted these times and events on a blank piece of paper so I could visualize the structure of the day and the time between significant events.
You may need to construct more than one template if your child’s school schedule changes from day to day (Phys. Ed happens at a different time on MWF than on TR, for example; or the schedule runs in a 6-day cycle, where timing on Day 1 is different from Day 2, etc).
Next you may want to figure out where your child’s blood glucose may be in question, and, therefore, when blood glucose checks are best conducted.
Tip from the Trenches
In our case, though our Care Plan stated that our son should check his blood glucose before snack, and before and after gym class, in reality gym was scheduled very soon after the start of the school day; since there was little to be gained by checking blood glucose before gym, we scrapped a “before gym” BG check. Further, the end of gym coincided with the start of snack time, so only one BG check was needed to cover both scenarios (post-exercise and pre-snack blood glucose). We also added a BG check before lunch, and the morning schedule was complete.
Then, looking at the afternoons on a typical day, the jotted schedule showed a time gap between the end of lunchtime and the end of the school day, so we scheduled a BG check for the midpoint: 2pm.
~Michelle
Potential Problems
You may then want to take a second look at a typical day, walking through it in your mind to anticipate when trouble spots may occur. When and where might your child need access to her monitor? When might she need to take a low treatment? Where could necessary supplies be stored for ease of access? Once you have identified potential issues, discuss possible solutions with school staff.
Tip from the Trenches
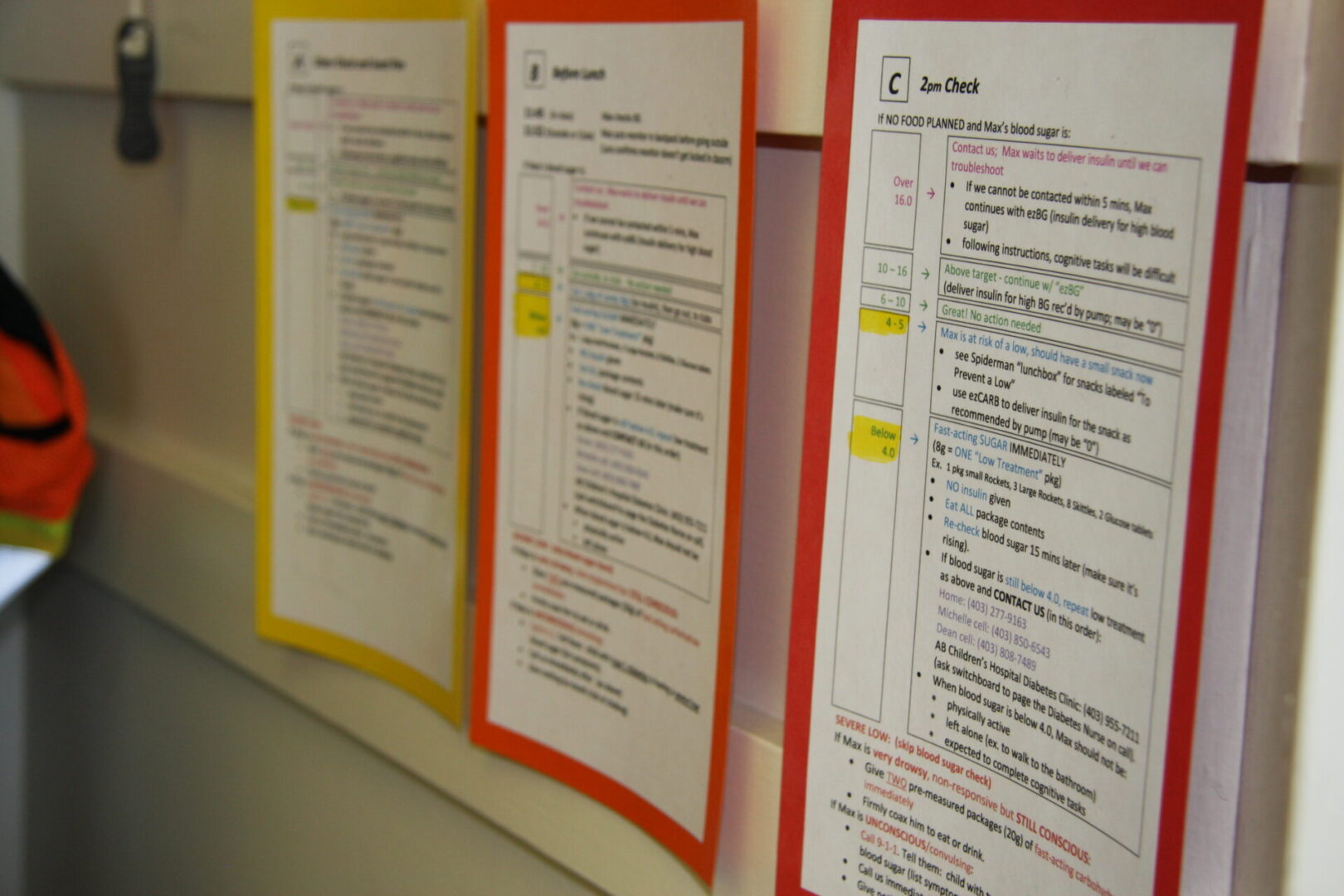
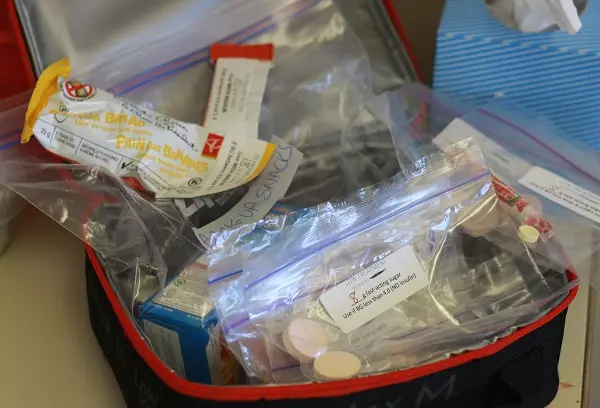
Because there are communal tables (rather than individual desks) in our son’s classroom, his teacher set up a small desk as a station for all his diabetes needs. (If your child has an individual desk, she may choose to store her d-supplies there.) At this station, he keeps a basket with his monitor, a timer for low treatment follow-ups, a Kleenex box for wiping any excess blood from his finger after BG checks, and a set of laminated instruction cards for his teacher and any other caregiver who may step in when she’s absent. Here they also store his Diabetes Kit – a lunch box containing an extra meter, back-up snacks to avoid a low, and premeasured packages of candy to treat lows. Each of the food items is labeled as to its purpose (“Low Treatment” or “Back up Snack to Prevent a Low”), with the carb count indicated.
~Michelle

You may also want to consider where your child could be when he experiences a low, so that low treatments may be stored at that location. Perhaps there could be a “stash” in the gym, the library, or the main office (with locations known by key adults, as well as your child).
Tip from the Trenches
At our son’s school, there are small packages of candy (enough to treat six lows) labeled with his name and their purpose (“Low Treatment”), and then stapled into the emergency files in each room; in the unlikely event of a school lockdown, his immediate needs will be covered anywhere in the school.
~Michelle
Communication
Often the most important factor for successful diabetes management at school is the quality of communication between home and school. In order for you to troubleshoot and adjust procedures effectively as needed, there needs to be a reliable system for parents to communicate with school staff, and for the school to communicate with home. This may include a written communication system, such as the Agenda booklets that many schools use for all of their students, as well as a verbal communication system when needed: Which phone number does the school call if they need to contact you quickly? Who should you contact at the school, and how do you get a hold of them? Some students with diabetes have their own cell phone with which they may communicate directly with their parents if they need support during the school day (you may choose to establish a rule that this phone is to be used for diabetes-related issues ONLY). Some parents and teachers text each other on their cell phones. Others use email. There are many options for communication – the key is discussing with school staff which option seems most appropriate in your situation.
In order to track blood glucose patterns during the school day, you (or the school, for record-keeping reasons) may want to keep a log of when blood glucose checks were done, and what the result was. If this is the case, you may want to discuss who will be responsible for writing in this log, how often it will be reviewed, and how you will be able to access it when needed. (Will it go home every day in your child’s backpack? Will it be an online record?) This record may be less important if your child wears an insulin pump with integrated blood glucose meter, as the pump history will automatically keep a record of blood glucose checks and insulin delivered.
To communicate the carbohydrate content of snacks and lunches brought from home, we have found it useful to stick a carb label on food containers, or in our son’s blood glucose meter (where he will need it right after his pre-lunch BG check, to input the lunch carbs into his pump). Whether you count the carbs for your child, or your child counts his own carbs, a label is a convenient reminder of the carb content.
Large dot stickers (like those often used for pricing at garage sales) are handy – just jot the number of grams of carbs and stick one on each food item. Or rectangular file labels, which are the medium of choice in our home, can be preprinted with:
For a printable carb label template:
Fine-Tuning the Plan
Now that you have a day-to-day plan implemented, you may find that there are some unanticipated issues within your child’s school day. You may find that you have to fine-tune the initial plan to better suit the new realities of which you have become aware. Both parents and school staff should feel comfortable with bringing forward their observations and suggestions – either at a pre-arranged semi-formal meeting time, or through any of the day-to-day communication channels you already have in place (text, phone, email, agenda books).
It’s okay if things don’t work as well as you planned initially. Through a continuing process of communication and fine-tuning, your child’s school days are bound to improve over time.
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE