You Have Arrived!
At Your Destination: tips for families traveling with the diabetes dragon
You’ve successfully navigated preparing, packing and travelling with type 1 diabetes... your family has arrived safe and sound. Now what do you need to know to smooth the path at your destination?
Travel can be stressful for anyone; travelling with diabetes can add additional worry. But with a little advance planning and prep, you can prevent common pitfalls and have a great, stress-free time away from home. Here are a few tips to reduce diabetes-related hassles once you've arrived at your travel destination:
Less Insulin? More Carbs?
If your holiday involves more exercise or activity than usual, you may need to lower your child’s insulin and/or give extra food. (For more information, see Managing Blood Glucose Before, During and After Exercise.) Conversely, the adrenaline response to an exciting trip may mean that you have to provide more insulin (basal and/or bolus). Look for trends and adjust accordingly.
Tip from the Trenches
I didn’t have to look very hard for trends on a recent road trip from Alberta to B.C. Within a few hours of leaving home, our son’s blood glucose climbed to the high teens and stayed there, despite numerous corrections, until we increased the basal rate on his pump by 20%. Once we did so, his blood glucose was much easier to keep in range.
Update: Now that my son is in his teens, we find that any temp basal less than 40% doesn't make much of a dent in avoiding highs due to inactivity.
~Michelle
Sickness & Infection
- If travelling to a country with potentially unsafe drinking water, you may choose to bring medication to stop diarrhea, as well as water purification tablets. It’s wise to drink only bottled water and either avoid fresh vegetables (which may be washed in dirty water) or peel them, if possible.
- Have a plan to manage sickness. (See Illness Management summary on this website.) Knowing how much extra insulin to give for high blood glucose and ketones, and how to lower insulin for low blood glucose and vomiting, will empower you to manage the unexpected while traveling. In the case of vomiting and/or diarrhea, stopping insulin may quickly lead to uncontrollable high blood glucose ketones. Check blood glucose often and give sips of drinks containing sugar (regular pop, juice, or tea with sugar). If vomiting and diarrhea continue, seek medical help.
- Reduce the risk of infection from injury (which may wreak havoc with blood glucose) by having your child wear cotton socks and shoes that fit well, and avoiding going barefoot. Carry sunscreen and a first aid kit containing Moleskin™ (for blister prevention). If injury occurs, monitor it closely and get medical help right away if it becomes infected.
- Once you have arrived at your destination, check where the nearest hospital is located and learn how to get emergency help. If you are in a large overseas city, seeking medical help at a university hospital is a good bet, as they often provide the most sophisticated medical care available.
Other Tips:
- Consider making reservations at restaurants to avoid long waits.
- If your child stays well-hydrated, it will be easier to manage high blood glucose, and to “flush out” ketones should they develop as a result of high blood glucose.
- Insulin will keep for one month at room temperature. If you are away for a month or less, you don’t need to worry about keeping the insulin chilled during travel. However, you do need to be careful that insulin is not exposed to extremely high or extremely low temperatures. If travelling by plane, you can avoid the extreme low temperatures in the cargo area of the plane by NOT PACKING INSULIN IN CHECKED BAGGAGE. If you are travelling by car, you can avoid exposure to very high temperatures by storing the insulin in an insulin wallet (Frio®) or a wide-mouth thermos bottle with an ice cube. Check the insulin often while travelling: if it has crystallized, clear insulin has become cloudy, or cloudy insulin has become lumpy/will not mix/frosts the inside of the bottle, it is best to DISCARD IT. (More on Storing Insulin.)
- Make sure your child wears his or her medical ID bracelet, or other medical identification.
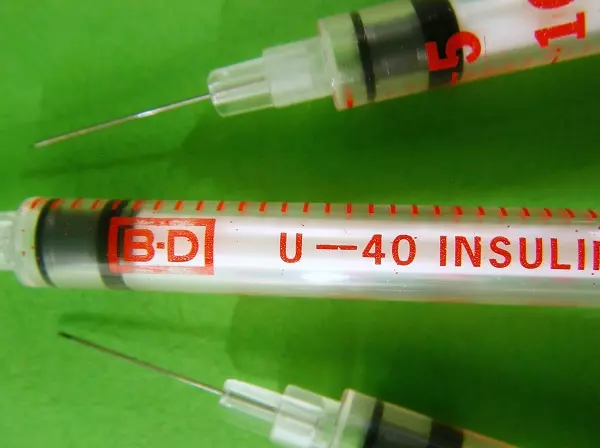
- Be aware of insulin concentration if you purchase it in another country. Canada has U-100 insulin and U-100 syringes. Some countries have U-40 insulin which must be used with U-40 syringes. If you buy insulin away from home and it is U-40, buy U-40 syringes, too. (If you use U-40 insulin with your U-100 syringes, you will get the wrong dose!) If your child uses an insulin pump and you think you may not be able to obtain U-100 insulin in your extended travels, before you leave have your health care team prepare you for the use of different concentrations of insulin.
The above information was significantly modified with permission from The Alberta Children’s Hospital Diabetes Clinic information handouts.
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE