Fat & Protein: prevent post-meal BG spikes
Michelle MacPhee
D-Mom & Creator/Co-founder of WTD
We know about how carbs raise blood sugar, but the impact of protein and fat can be significant, too. What can we do to avoid the post-meal spikes associated with the intake of fat and protein? How much additional insulin do we need? How/when do we deliver that insulin to match the delayed effect of fat? Here we discuss a method for bolusing for fat and protein, outline its pros and cons, and then share how our family adapted the process to maximize time in target.
Background info for this article:
As I shared in Our Family's D-Revolution: 3 Keys to Managing BG & Food, in the first several years after our son was diagnosed with type 1 diabetes at just over a year old, I came to dread (and actively avoid!) a frozen treat on a hot summer day, Friday Family Pizza Night, or an afternoon at the Play Place, munching on fries. All because of the price we would pay later in huge BG spikes, in repeated correction doses that didn't work, in frustration and anxiety. Yet I struggled with the idea that my son was missing out on these typical kid treats. I resented the idea that our family’s activities were being controlled by diabetes. Then we learned about the concept of Fat Protein Units and our family's quality of life improved dramatically.
Which foods are high in saturated fat?
These are some of the high-fat foods that our family "fat boluses" for (gives extra insulin to prevent post-meal BG spikes):
- Pizza (the more cheesy the pizza, plus the greater the number of high-fat meat toppings, the more saturated fat it contains. For eating out, this varies greatly from restaurant to restaurant. In our experience, Boston Pizza tends to use much less cheese compared to Panago, and thus is lower in saturated fat, resulting in relatively less insulin resistant post-meal.)
- Burgers
- Nachos (the tortilla chips and the cheese may have a high fat content)
- Cheese buns (sometimes - depends on what type and how much cheese is used)
- Fatty processed meats (such as sausages, pepperoni, bacon, some packaged hams)
- Creamy sauce (those made with heavy cream or lots of butter - think Fettucine Alfredo)
- Rich cheesecake (the full-on, high-fat variety)
- Desserts made with real whipping cream
- Ice cream made with heavy cream; ice cream treats/bars (like Magnum, Hagen Daaz or Klondike bars)
- Chocolate bars (sometimes)
- Peanuts
- Foods/desserts made with lots of butter
- Foods fried in shortening, lard or bacon grease (which could include French Fries, Hashbrowns, Deep-Fried Fish, etc)
- Potato Chips, Nacho chips (like Doritoes)
The Warsaw Approach A Method for Dealing with Fat and Protein
Listen to a podcast:
I recently recorded an episode of Juicebox Podcast with d-dad Scott about this exact topic... I love his podcast! He's super-intuitive with diabetes-care, has great stories, and he lives with the dragon, so he GETS IT! For episode #471 we talked about Five Guys and A&W (yum), making your own potato chips, thinking in pictures (or not), pulling a number out of the air, being exactly where you're supposed to be, and how the fat in foods leads to crazy post-meal spikes... UNLESS you bolus insulin for fat. Here's where you can listen for free:
(Let’s all show him some love with a download and a positive review!)
Apple Podcasts
Spotify
Amazon Music
Google Podcast
Online: Juicebox Podcast
The Warsaw School Program for Dosing Mealtime Insulin proposes one approach for avoiding post-meal high blood glucose due to intake of fat and protein; it's widely used by patients with insulin-dependent diabetes in Poland and Germany.
In addition to bolusing for carbohydrates just as we do here in Canada (by counting carbs and using a Normal Bolus to deliver insulin according to an individualized I:C ratio), the Warsaw School advocates an additional bolus for protein and fat, given as an extended bolus.
- The duration of this extended bolus is determined by the amount of protein and fat in the meal.
- The amount of protein and fat in the meal is expressed in “Fat-Protein Units” (FPU).
- One FPU is equivalent to 100 kcal of fat or protein, and has a blood-glucose-raising effect equivalent to 10g of carbs.
From those basics, the Warsaw School approach outlines a systematic, precise process for calculating the additional insulin that may be needed to cover the fat/protein content of a meal: a low-protein/low-fat meal would call for little to no extra insulin; more insulin would be required for a high fat and/or high-protein meal.
To reduce post-meal BG spikes caused by fat and protein:
give insulin for carbs
PLUS
give insulin to cover the fat and/or protein
1 FPU =
100 kcal of fat or protein
—————
1 FPU raises BG ≅
10g of carbs
The Process
After giving a normal bolus to cover the carbohydrates, the extra insulin (amount and duration) to cover fat and protein is calculated using Fat-Protein Units (FPU’s) as in the example that follows. However, there are a few important notes before we get started:
- If it ain't broke, don't fix it. If you're not currently struggling with high BG spikes after meals, then you don't need a fat/protein solution! This could be because your family eats a consistent amount of fat from day to day (lots or a little), so your basal rates and carb ratios already account for fat and protein.
- Stick with me... it may look daunting! but it will make sense by the end of this example.
- Keep in mind that the effect of protein is included in this approach, despite what some consider controversy regarding the effect of protein on BG (as discussed in How Fat and Protein Affect BG).
- One of the drawbacks of this approach is that patients in the population that often uses this method have what many would consider an unacceptably high rate of hypoglycemia (low blood sugar). So it may be risky to follow this method exactly as outlined in the first example. Read through to the end to learn about my suggested adaptations (that our family uses) to reduce the very real risk of lows!
- Also note is that this process is not currently considered best practice within the Clinical Practice Guidelines set out by the Canadian Diabetes Association. So, according to Canadian health care professionals, it may be risky to follow this method as outlined in the first example.
- As always, “Your Diabetes May Vary”! There are individual differences in how different bodies process carbs, fats and protein, as well as differences in portion sizes, food items, amount of exercise already completed and planned, hormones, body types, stress levels, illness, etc. So it is wise to use the general principles outlined here within the context of your own situation, and CONSULT YOUR DIABETES HEALTH CARE TEAM if you would like to implement these principles within your own/your child’s blood glucose management program.
Let's go through an example calculation together:
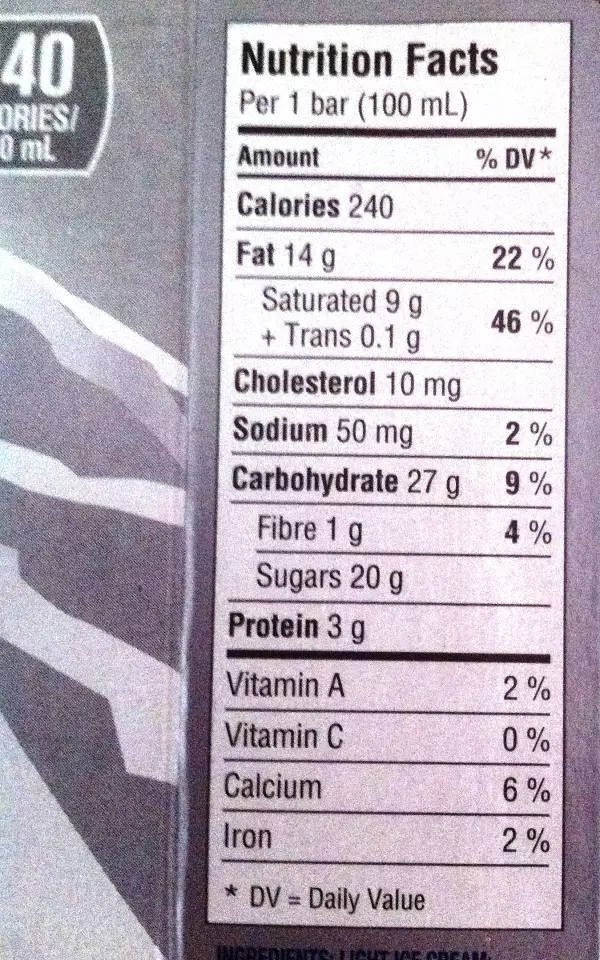
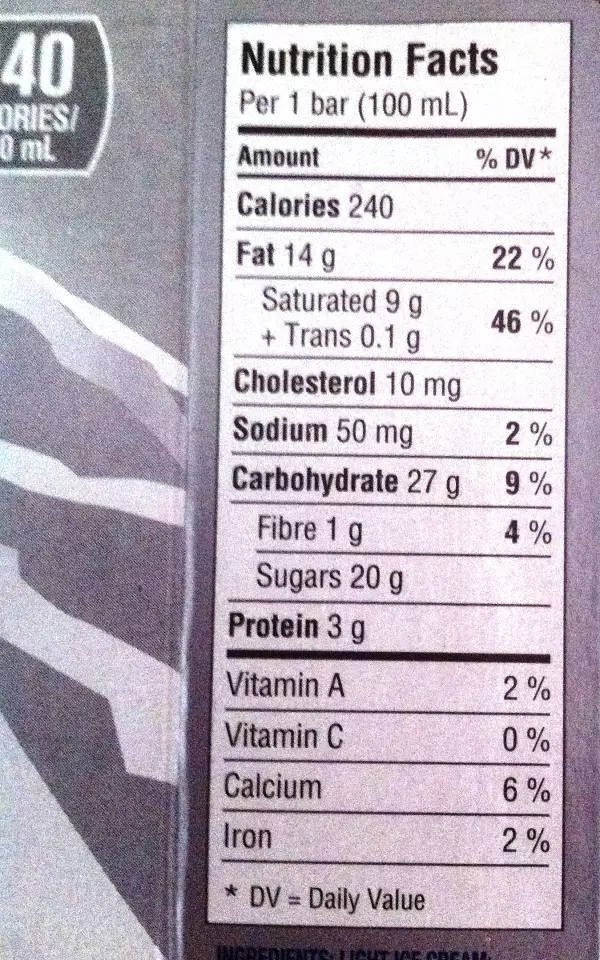
For simplicity, we will consider a single fat- and protein-containing food item, a Klondike® Kandy Bar™ chocolate-coated ice cream treat.
After giving a normal bolus for the carbs, as usual (which in this case is 26g of carbs, from the package label, below) I would:

1. Identify how much fat & protein the food contains.
We start by finding out the number of grams of fat and the number of grams of protein. We can get this information from a nutrition facts label, or by using a nutritional scale, or by accessing a food database (app, book, or website, for example). If your meal includes more than one significant source of fat and/or protein, you can add up the fat and protein values from each of the different foods, and then work with those totals according to the same process.
Example:
From this food label, we learn that one Kandy Bar has 3g of protein and 14g of fat.
2. Convert into units of energy.
Next we multiply the grams of protein by a factor of 4, and the grams of fat by a factor of 9, to determine the amount of energy (in kcal) contributed by each.
kcal from protein = Protein (in grams) x 4 kcal/g
and
kcal from fat = Fat (in grams) x 9 kcal/g
Why 4 (or 9)? That’s simply the mathematical relationship between grams of fat (or protein) and kilo-calories: there are 4 kcal of energy in 1 gram of protein, and 9 kcal of energy in 1 gram of fat.
Example:
For protein:
kcal from protein = Protein (in grams) x 4 kcal/g
When we plug our nutrition label facts into that formula: 3g of protein x 4 = 12 kcal,
we learn that the 3g of protein in our Kandy Bar contributes 12 kcal of energy.
For fat:
kcal from fat = Fat (in grams) x 9 kcal/g
When we plug our nutrition label facts into that formula: 14g of fat x 9 = 126 kcal,
we learn that the 14g of fat in our Kandy Bar contributes 126 kcal of energy.
3. Calculate the Total Calories.
Next we add these two together to get the TOTAL calories from protein and fat combined.
kcal from protein + kcal from fat = TOTAL kcal from Fat and Protein
Example:
kcal from protein + kcal from fat = TOTAL kcal from Fat and Protein
12 kcal from protein + 126 kcal from fat = 138 total kcal (from fat & protein combined)
4. Calculate Fat-Protein Units.
Now that we have the total energy (in kcal), we need to calculate the number of Fat-Protein Units (FPU). Since there are 100 kcal of energy in 1 FPU (as we mentioned in the introduction to this article), we calculate FPU by dividing the total kcal by 100 kcal per FPU:
FPU =
total kcal from fat and protein
100 kcal/FPU
Example:
From step 3 we know that we have a total of 138 kcal in our Kandy Bar. When we divide that by 100, we get:
138 kcal ÷100 kcal/FPU
= 1.38 FPU, or
= 1 FPU (rounded to nearest full unit)
5. How long is the extended bolus?
Now that we know how many FPU we are dealing with, we use that number to determine the duration of the extended bolus (i.e. how long to extend the insulin bolus for fat and protein), according to the following chart (provided by those who developed the Warsaw method):
for 1 FPU, program the extended bolus over 3 hours
for 2 FPU, program the extended bolus over 4 hours
for 3 FPU, program the extended bolus over 5 hours
for 4 FPU, program the extended bolus over 8 hours
Example:
For one Kandy Bar (which contains 1 FPU), we will extend the bolus over 3 hours.
6. How much extra insulin is needed?
The last thing we need to do is figure out how much insulin to deliver (for fat and protein) in that extended bolus.
To calculate the amount of insulin (in units), we multiply by 10 (because the BG-raising power of 1 FPU is equivalent to 10g of carbohydrate, as we mentioned in the introduction to this article). This gives us a carb-equivalency (that is, the amount of carbs that would raise BG by the same amount as the fat and protein in our Kandy Bar will). We then divide those "pseudo-carbs" by your (individualized) insulin-to-carb ratio for that time of day (just as you normally would do to figure out how much insulin to give for carbs):
units of insulin =
FPU x 10g ‘Carbs’ per FPU ÷ I:C ratio
* This number “10” in the formula can be changed to decrease the amount of extra insulin given to cover fat, if needed. See Tips from the Trenches below.
Example:
In step 4 we determined that our Kandy Bar contains 1.38 FPU. When we plug that into this formula (with an Insulin-to-Carb Ratio of 1:6, which is my son's I:C ratio for supper*) we get:
* Note: Your I:C ratio will likely be different!
1.38 FPU x 10g ‘Carbs’ per FPU ÷ 6 carbs/unit
= 2.3 U of insulin in the Extended Bolus
We can round this to the nearest half-unit for injections (= 2.5 units), or
We can round this to the nearest 0.05U for insulin pumps, which in this case is no change (= 2.3 units)
The End Result
To make a long story short:
In this example, to cover the fat and protein when my son has a Kandy Bar after supper:
I would first give the usual bolus for carbs before he starts eating.
Then later I would deliver an extra 2.3U of insulin in an extended bolus over a duration of 3 hours.
When is "later"? Because the effect of fat is delayed, we don't give the "fat bolus" before, or right after, he eats; instead we wait 1-2 hours after he's finished eating to start the extended bolus. The amount of time that we wait depends on the amount of fat (1 hour for a small amount of fat; 2 hours for large amounts of fat).
SHARE THIS PAGE
HOWEVER…
… as we mentioned, one problem with this method is an unacceptably high risk of hypoglycemia (low blood sugar). When I used the FPU concept exactly as outlined above to deal with high fat meals such as chicken nuggets and fries, ice cream, or pizza, my son’s BG went low (sometimes very low!) every time.
To reduce this risk and keep our kids safe, I suggest some adaptations to the above process that result in more conservative insulin dosing. In other words, when you use the adaptations, less insulin given is given, so the process is safer.
ADAPTED WARSAW APPROACH:
Tips from the Trenches
ADAPTATION #1
First, because Gary Scheiner talks about the fact that protein has little effect on BG when consumed with carbs, and because my son almost always has carbs when he eats protein, I dropped the Protein portion of this process entirely. I calculate the amount of Fat Units, and use that alone to determine the amount and duration of the extended bolus.
In practical terms, this means I use Zero for grams of protein in the calculations. (See the example that follows under Adaptation #2.)
Tips from the Trenches
ADAPTATION #2
In addition, I play with the amount of ‘Carbs’ per FPU, given above as 10; usually I multiply the FPU’s instead by 9. This is like saying that the fat in the food raises blood sugar like 9g of carbs would (rather than 10), which assigns less BG-raising power to the fat contained in that food. Sometimes I multiply by even less: 8 "pseudo-carbs" (which reduces the insulin dose even further), especially when my son has been very active that day, and is therefore more insulin-sensitive.
Example of the ADAPTED (More Conservative) Process:
Using the same Kandy Bar example above, after giving a normal bolus for carbs, I would:
1. Identify how much fat the food contains.
Example:
From this food label, we learn that one Kandy Bar has 14g of fat.
2. Convert into units of energy.
Next we multiply the grams of fat by a factor of 9, to determine the amount of energy (in kcal) contributed by fat (and only fat, since we are counting out any impact of protein in the more conservative approach).
kcal from fat = Fat (in grams) x 9 kcal/g
Example:
For fat:
kcal from fat = Fat (in grams) x 9 kcal/g
When we plug our nutrition label facts into that formula: 14g of fat x 9 = 126 kcal,
we learn that the 14g of fat in our Kandy Bar contributes 126 kcal of energy.
3. Calculate the Total Calories.
We skip any calculations for this step in the adapted process. Since we did not include protein, the total kcal is equal to the total grams of fat alone.
Example:
total kcal = kcal from fat = 126
(same number as in step 2)
4. Calculate Fat-Protein Units.
Now that we have the total energy (in kcal), we need to calculate the number of Fat Units. Since there are 100 kcal of energy in 1 Fat Unit, we calculate Fat Units by dividing the total kcal by 100 kcal per Fat Unit:
Fat Units =
total kcal from fat
100 kcal/fat unit
Example:
From step 2 we know that we have a total of 126 kcal from fat in our Kandy Bar. When we divide that by 100, we get:
126 kcal ÷100 kcal/FPU
= 1.26 Fat Units, or
= 1 Fat Unit (rounded to nearest full unit)
5. How long is the extended bolus?
Again we look to the chart to determine the duration of the extended bolus:
for 1 FPU, program the extended bolus over 3 hours
for 2 FPU, program the extended bolus over 4 hours
for 3 FPU, program the extended bolus over 5 hours
for 4 FPU, program the extended bolus over 8 hours
Example:
For one Kandy Bar (which contains 1 FPU), we will extend the bolus over 3 hours.
(No change from the first example.)
6. How much extra insulin is needed?
The last thing we need to do is figure out how much insulin to deliver for fat in that extended bolus.
In this adapted example, instead of multiplying by 10, we will multiply by a more conservative 8 (which is like saying that the BG-raising power of 1 FPU is equivalent to 8g of carbohydrate). We then divide those "pseudo-carbs" by the insulin-to-carb ratio for that time of day:
units of insulin =
FPU x 8g ‘Carbs’ per FPU ÷ I:C ratio
Example:
In step 4 we determined that our Kandy Bar contains 1.26 Fat Units. When we plug that into this formula (with an Insulin-to-Carb Ratio of 1:6, which is my son's I:C ratio for supper*) we get:
* Note: Your I:C ratio will likely be different!
1.26 FPU x 8g ‘Carbs’ per FPU ÷ 6 carbs/unit
= 1.68 U of insulin in the Extended Bolus
We can round this to the nearest half-unit for injections (= 1.5 units), or
We can round this to the nearest 0.05U for insulin pumps (= 1.7 units)
The End Result
To summarize, using the ADAPTED Warsaw School approach,
In this example, to cover the fat when my son has a Kandy Bar after supper, I would deliver 1.7U of insulin in an extended bolus over a duration of 3 hours. (In addition to the usual carb bolus of insulin that was given before he started eating.)
I would start the extended bolus 1-2 hours after he eats, depending on the amount of fat. In this case, I would likely start the extended bolus 1 hour after eating.
Compared to 2.3U in the first example above, the 1.7U calculated in this adaptation presents a more conservative version of the Warsaw School program; one that we have found works GREAT in most cases for our son (check out some comparative BG data from our family’s experiments with FPU).
Although this may not seem like much of a change in insulin dose, it made a huge difference in our real life - it meant the difference between persistent lows and in-range BG for our school-age son.
Also, the gap between the 2 methods gets even larger when a large amount of fat is eaten (compare the 14g of fat in a Kandy Bar used for these examples, to the 57g of fat (!!!) in a McDonald's McChicken sandwich and poutine. The amount of extra insulin for fat grows exponentially.)
Other Ways to Adapt the Process
On an ongoing basis, our family "adapts" the Warsaw method to best match the conditions of the day:
- if our son was more active than usual, we use a lower carb-equivalency factor (8)
- towards the end of a school break (like spring vacation) he tends to be less insulin sensitive due to the lower level of activity, so we use carb-equivalency factor of 10 at those times
- we make the extended bolus shorter or longer based on past experience with certain foods and how quickly they impact blood glucose
- we add more insulin for very high amounts of fat, as we've found that double the fat requires more than double the insulin in our son's case
- if this is the second high-fat meal in the day (think nachos for lunch, then burgers and fries for supper) then we add more insulin for the second meal, as the insulin-resistance due to fat is compounded
SHARE THIS PAGE
Tips from the Trenches
We are still conscious of the risk of lows and check his BG often after using this more conservative formula; we find that around the 4-6 hour mark is when his BG may dip too low, so clearly we still have some tweaking to do, perhaps in terms of the duration of the extended bolus. We have had to bring in a low treatment at this point on more than one occasion, so I caution you to be vigilant with checking your child’s BG, especially before you have a good idea of the effect of this approach on his/her individual body. But that said, given that we are willing to be vigilant, we have found this approach to be a huge benefit to our family!
Tips from the Trenches
We guesstimate the amount of insulin and the duration of the extended bolus for FPU of 5 or more (as these exceed the numbers given in the chart). That 57g of fat at McDonald's translates to 5.1 Fat Units; we've had success with setting an extended bolus of 12 hours in that case. And there are times our son has had the equivalent of 8 Fat Units in a single meal (that's 88g of fat!). In all cases, we just do our best and watch his BG closely over the next several hours.
Tips from the Trenches
At first I found this calculation to be cumbersome, and if I didn’t happen to have my FPU Worksheet with me when we wanted to get ice cream on an outing, then I was left with the same “by guess and by golly” approach that I had used before I learned about this concept. So I condensed the calculations (individualized for our son’s needs) into fewer steps and stored the shortened form on my phone for easy access on the go. Here is how I condensed the formula into fewer steps:
(Remember that this abridged form takes into account only fat – not protein – since this is what works for our son. You may need to come up with your own short hand to accurately reflect your child’s individual needs.)
Step 1: Calculate Fat Units = grams of Fat x .09
This number tells me the duration of the extended bolus.
14 x .09 = 1.26 –> extend bolus for 3 hours
Step 2: Calculate the Insulin Dose:
Fat Units x 8g ‘Carbs’ per FPU ÷ I:C ratio
(Our son's I:C = 1:6 for most of the day)
= Fat Units x 8 ÷ 6 = Units of extra insulin needed
1.26 x 8 ÷ 15 = .67U = .65U (rounded)
All I have to remember on the go is:
Fat x .09 x 8 ÷ I:C
Tips from the Trenches
From Danielle:
My son responds differently than Michelle’s when it comes to fat digestion! What I have found with Paul (after many years of trial and error) is that fat doesn’t seem to fully affect him until at least 6 hours after he eats it AND when I tried this approach as outlined above, his BG tanked at the 4 hour mark, so he needs insulin up front only for the carbs (needs the extra insulin to cover fat much later). I find the “pizza solution” to work better for him but it sure isn’t a spelled-out approach (like the above example). I still need to experiment more with possibly using a modified FPU approach. I would try using the amount of carbs and time guidelines found above (using the Fat Protein Unit calculations) and use it instead of a temporary basal rate increase 6 hours later in order to have a more mathematical approach.
And One Last Tip from the Trenches
From Michelle:
I have asked myself often, “What counts as ‘high fat’?” and though I still can’t answer that question in a precise way, we have found in our family that we don’t need to use this method for meals below 10g of total fat. That threshold may be higher or lower for other people with type 1 diabetes.
The Bottom Line
In most cases, this approach works very well for our family, helping to prevent post-meal blood glucose spikes and eliminating the frustration of soaring blood glucose. It’s enough to convince us to continue using an adapted Fat-Protein Units approach!
For other examples of dealing with fat and protein, illustrated with actual BG results:
We gratefully acknowledge the information provided by Lorraine Anderson (RD, CDE, Senior Clinical Manager, formerly of Animas Canada) and Shannon Cassar (RN, CDE, Alberta Children’s Hospital Diabetes Clinic), which served as the basis for this article. Without you, we might never had experienced this diabetes management revolution! Thank you!
The above information was reviewed for content accuracy by Lorraine Anderson, RD, CDE.
SHARE THIS PAGE