Checking & Adjusting Basal Rates MDI
Adjusting Insulin (MDI): testing & tweaking basal rates
Basal insulin is the background insulin which, at the correct dose, keeps blood glucose steady in the absence of food and exercise. But how can you tell whether the current basal insulin dose is working well or not? Here we look at how to assess the current basal dose in a Multiple Daily Injection (MDI) program, then we outline in detail the process of fine-tuning basal insulin - including the reason why we should check blood sugar in the middle of the night.
Before Reading This Article...
If you have not done so already, we recommend that you read the following WaltzingTheDragon.ca pages on insulin adjustment within Basal-Bolus/MDI programs as background for the information that follows:
Basal Insulin
Basal insulin is the background insulin which keeps blood glucose steady in the absence of food and exercise. A healthy pancreas secretes a small amount of basal insulin into the bloodstream every few minutes, to match the small amounts of glucose released by the liver on a continuous basis, so that glucose can be used by the body’s cells for basic energy needs. For a person with type 1 diabetes on a Multiple Daily Injections (MDI) program, basal insulin is delivered as long-acting “peakless” insulin, such as Lantus® or Levemir®.
Basal insulin needs vary from person to person, and across the lifespan. Adults and adolescents typically need more basal insulin in the early morning hours to deal with the release of hormones involved in waking (known as the Dawn Phenomenon). Children often need more basal insulin in the late evening hours to deal with the release of growth hormones a few hours after they fall asleep.
Initial Basal Doses
When your child is first diagnosed, her doctor should determine an initial dose of basal insulin that is appropriate for your child’s age, growth stage, and activity level. As she grows, changes will need to be made to these basal insulin doses. Periodically, you may want to test/verify how well the existing basal insulin doses are meeting her current need for insulin. You could then use the results as a basis of discussion with your child’s diabetes health care provider.
Fine-Tuning Basal Doses
Since basal insulin (Lantus® or Levemir®) is supposed to keep blood glucose steady in the absence of food, exercise and bolus insulin, if your child is on an injected insulin program, a good indication of whether or not the current basal dose is accurate is whether blood glucose remains steady overnight (when these factors are absent for longer periods). As such, if your child’s basal dose of insulin is correct, his blood glucose should not vary by more than 2.0 mmol/L from bedtime to waking the next morning (presuming that the conditions outlined below are met).
If you choose to check your child’s current basal dose overnight:
1. Have him eat a healthy supper, avoiding high fat food and restaurant/takeout food. Fat affects blood glucose by causing it to rise over several hours, thereby confounding test results.
2. Have him engage in no more than the usual amount of exercise before bedtime. Limit activity to moderate intensity and duration. Physical activity affects blood glucose by lowering it for up to several hours afterward.
3. Until the next morning, have your child refrain from eating/drinking anything other than water and diet drinks (0 calorie, 0 carb). Even low carb foods and protein can affect blood glucose, thereby confounding the test results.
4. Check blood glucose 3 hours after supper*.
- If the reading is 4.0 mmol/L or less, stop the test and treat the low as usual. You’ll need to wait until another night to test basal rates. (And this may indicate a need to adjust the supper I:C ratio, if this is not an isolated incident.)
- If the reading is 14.0 mmol/L or greater, stop the test and give the usual correction for the high blood glucose. You’ll need to wait until another night to test basal rates. (Again, this may indicate a need to adjust the supper I:C ratio, if this is not an isolated incident.)
- If the reading is between 4.0 and 14.0 mmol/L, proceed with the basal test as outlined in the steps that follow.
5. Check blood glucose again midway through your child’s sleep time* (responding as above if blood glucose is below 4.0 or greater than 14.0).
6. Check blood glucose again when your child wakes up*.
*Times to check blood glucose:
If your child finished eating at 6 pm, you could check blood glucose at 9 pm, 2 am, and 7 am, for example.
7. Assess the test results:
- If blood glucose stayed steady (within 2.0 mmol/L from bedtime to waking), no changes to the basal dose are likely needed at this time.
- If blood glucose dropped more than 2.0 mmol/L from bedtime to waking:
You may choose to decrease the basal dose of Lantus® or Levemir® (by 10%, for example) and repeat the test on the next possible night.
For example, if the bedtime reading was 9.5, middle of the night reading was 8.5, and morning reading was 6.0, and your child’s current dose of Lantus is 6.0U, you could subtract 10% to arrive at 5.4U, round off to 5.5U, and repeat the test with a basal dose of 5.5U.
- If blood glucose rose more than 2.0 mmol/L from bedtime to waking:
You may choose to increase the basal dose Lantus® or Levemir® (by 10%, for example) and repeat the test on the next possible night.
For example, if the bedtime reading was 9.5, middle of the night reading was 11.0, and the morning reading was 12.0, and your child’s current dose of Lantus is 6.0U, you could add 10% to arrive at 6.6U, round off to 6.5U, and repeat the test with a basal dose of 6.5U.
Why Check Blood Glucose in the Middle of the Night?
If we checked blood glucose at bedtime and at wakeup only, and found more than a 2.0 mmol/L rise, there are at least a few possibilities in terms of what happened overnight:
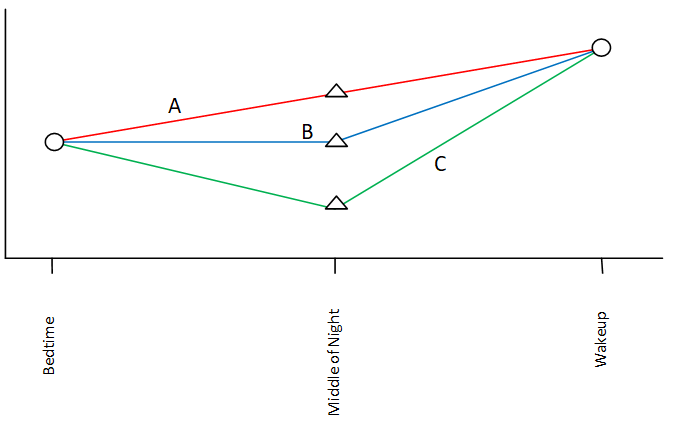
A. blood glucose may have risen steadily;
B. blood glucose may have stayed steady in the first part of the night, followed by a sharp increase in the latter part of the night; or
C. blood glucose may have dropped in the first part of the night and then rose sharply as a result of the preceding low blood glucose.
This last scenario is referred to as a “low rebound” (or, the Simogyi Effect): as a result of a low, the liver releases stored glucose (glycogen), resulting in high blood glucose later. In order to rule out an undetected low, it is essential to check your child’s blood glucose at least once midway through your child’s sleep time.
How we deal with the overnight rise in blood glucose depends on which of the above scenarios actually occurred:
- If blood glucose rose steadily overnight as in A: it makes sense to increase the basal dose (Lantus® or Levemir®).
- If blood glucose remained steady for part of the night and then increased towards morning as in B: you may choose to add a correction of rapid-acting insulin at the appropriate time, OR you could consider adding a bit of intermediate-acting insulin (N/NPH) at bedtime to mediate the problem.
- If blood glucose dropped and then rose as a result, as in C: then a decrease in the basal dose may actually result in lower waking blood glucose readings.
If you would like assistance with sorting out the possibilities, please consult your child’s diabetes health care team.
(If you’re a Type A personality like I am, during a basal test you may choose to do 2 checks in the middle of the night: 12 am and 3 am, for example. ~Michelle)
Next Steps on Adjusting Insulin in MDI:
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE