Lights! Camera! Insulin Action! NPH
Adjusting Insulin (N or NPH): how insulin action impacts blood glucose
If your child has predictable lows (or high BG), you may need to adjust their insulin doses. But which dose, and how much should you adjust by? You can start the process here by looking at how and when the action of N or NPH (intermediate-acting insulin) affects BG in a conventional insulin program.
Before Reading This Article...
Before making any changes to insulin doses, it is important to understand the action of insulin (the onset, peak and duration of different types of insulin). Therefore, as background for the information that follows, we recommend you first review Insulin Types & Action.
You may remember that:
- There are 3 general insulin programs:
-
- Conventional Program in which you give 3 injections of N/NPH and/or rapid-acting insulin
- Basal-Bolus Program with Multiple Daily Injections (MDI) in which you give 4 - 6 (or more) injections of long-acting plus rapid-acting insulin
- Pump Therapy program in which you infuse (rather than inject) rapid-acting insulin only.
On this page we are talking about a Conventional Program (#1).
- Your child's current blood glucose (BG) is a result of several factors, including the way that a particular insulin behaves, which we call "insulin action." In other words, insulin action describes how quickly the insulin starts to affect blood sugar, when it peaks (has the most power), and how long the effect of the insulin lasts.
- Intermediate-acting insulin (such as Humulin N® and Novolin NPH®, known as N and NPH for short) starts to work in 2-4 hours, peaks at 6-10 hours, and lasts up to 18 hours.
For the discussion that follows, “intermediate-acting” insulin refers to N or NPH; “rapid-acting” insulin refers to Humalog®, NovoRapid®, or Apidra.®
How Insulin Affects Blood Sugar in a Conventional Insulin Program
This insulin action diagram for a conventional insulin program shows that the blood glucose at a given time is affected by a certain previous insulin dose. If we follow the curve back from breakfast, for example, we can see that it leads to bedtime, when a dose of N/NPH was given. If we follow the rapid-acting curve back from lunch, we can see that it leads to breakfast.
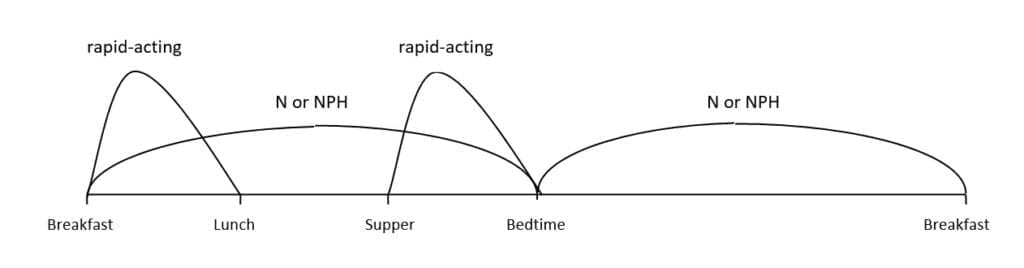
Another way of expressing this relationship is to say that:
-
Blood Glucose before breakfast tells you about how well the Bedtime dose of N or NPH is working.
-
Blood Glucose before lunch tells you about how well the morning dose of rapid-acting is working.
-
Blood Glucose before supper tells you about how well the morning dose of N or NPH is working.
-
Blood Glucose at bedtime tells you about how well the supper dose of rapid-acting is working.
Therefore, if the breakfast blood glucose is consistently out-of-range (either too high or too low), you may want to change the bedtime N/NPH. If the bedtime blood glucose is consistently too high, you may want to increase the supper dose of rapid-acting insulin. If the lunch blood glucose is consistently too low, you may want to decrease the morning dose of rapid-acting insulin.
Next Steps on adjusting insulin in a 3-injection Conventional Insulin Program:
The above information was adapted with permission from The Alberta Children’s Hospital Diabetes Clinic information handouts.
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE