Adjusting Insulin in a Pump Program: adjusting insulin based on blood glucose patterns
If your T1D child's blood sugar swings wildly, or is low at the same time each day (or high!) you may need to adjust insulin doses. But which dose, and how much? Looking for patterns in the numbers in your child's pump data is a great place to start. Here we'll show you what to look for and how to tweak things, using a semi-structured record review to adjust your programmed pump settings.
Before Reading This Article...
If you have not done so already, we recommend that you first read the following WaltzingTheDragon.ca articles as background info:
A Basal-Bolus Approach to Insulin Pump Therapy
How Insulin Action Impacts Blood Glucose in an Insulin Pump Program
Semi-Structured Record Review: a strategy to adjust insulin pump doses
A Record Review is a first-steps process of insulin adjustment which, in many cases, gives you enough information to make changes to insulin doses (thereby reducing blood glucose swings and unpredictability). That is, by structuring meals/snacks and keeping complete records for several days, you may get a pretty good idea of how well the current settings are working for your child (without more intensive methods of investigation such as strict basal testing).
Gathering Data To assess your child’s current pump settings over a week:
1. Food
Have your child eat three meals, at the regular meal times. Have them avoid carbohydrate-containing snacks and high-protein snacks between meals. If possible, have them forego a bedtime snack.
2. Keep a food record
Keep a food record in which you write down what your child eats during the assessment period. Include the amount of each food, the type (ex. white bread vs. whole grain bread), and the carb content.
3. Check blood glucose:
- before each meal
- 2-3 hours after each meal (and after the bedtime snack, if your child cannot skip this snack)
- at Midnight
- at 3 a.m.
4. On the pump log, record the following:
- Blood glucose (include the time blood glucose check was done)
- Carbs eaten (amount, at what time)
- Bolus insulin given for food (amount, at what time)
- Bolus insulin given for high blood glucose (amount, at what time)
- Note any exercise (time, type and amount)
- Note infusion set changes
5. Basal Rates
Keep track of basal insulin settings during this time (either by printing off a Pump Settings Report from the pump software, or by writing a list of basal rates throughout the day). Also note time and amount of any temporary basal settings.
6. Total Insulin
Check the pump history and record the total basal insulin, as well as the total daily dose of insulin, for each of the 7 days of the assessment period.
7. Look for BG Patterns
Review the pump data or log book every 3 days, looking for patterns of high or low blood glucose.
A. If blood glucose is below the target range at the same time of day, for 2 days in a row, consider a decrease in the programmed rate(s) which impact blood glucose at that time.
- Look for patterns of exercise, food consumption (high fat, low glycemic), or infusion set changes which may explain lows – it’s possible that these factors, not the programmed insulin doses, are responsible for the lows.
- It’s a good idea to adjust for low blood glucose first. This is because lows (especially severe lows) present a greater health risk in the short term. In addition, lows can cause high blood glucose readings later, so correcting the lows may also correct for some highs. Once you have low blood glucose under control, then adjust for highs.
- If there are 3 or more lows per week but no pattern, contact your diabetes health care provider for guidance.
B. If blood glucose is above target at the same time of day, for 3 days in a row, consider an increase in the programmed rate(s) which impact blood glucose at that time.
- It’s best to increase only one dimension at a time, and then wait 2 to 3 days before making other changes. This gives you a chance to assess the effects of the change.
- If there is more than one time of the day when blood glucose tends to be high, it helps to start by adjusting for the earliest one. This may resolve the problem of highs later in the day, too.
- If blood glucose readings are high across the whole day, it is most effective to start by adjusting for the morning blood glucose first. Make additional changes only after you have had a chance to see the effect this has on readings for the rest of the day.
Alternatively, an increase in basal rates may be needed. If you are unsure, check with your child’s diabetes health care team, or conduct a fasting basal test.
- If you often give corrections for high blood glucose, this may be an indication that an increase is needed in one or more of the programmed rates affecting blood glucose at that time (that is, basal rate, I:C ratio, and/or ISF; you may even need to adjust the DIA setting).
- Again, look for patterns of exercise, food consumption, and infusion set changes which may explain highs. For example, some types of exercise may involve the release of adrenaline which leads to insulin resistance; foods high on the glycemic index may cause higher post-meal BG spikes which take longer to return to target while low GI foods may cause an initial drop in blood glucose followed by a high later; if the infusion set has been in longer than recommended, insulin may not be absorbing properly. It’s possible that these factors, not the programmed insulin doses, are responsible for the highs.
How Do I Change Insulin Doses?
Based on the results of your assessment as outlined above, you may decide to make changes to the programmed rates and ratios insulin doses.
- Change one thing at a time. Then assess the resulting change on blood glucose patterns before making other changes.
- You may want to forward the records from the assessment period to your diabetes health care provider for their suggestions.
- If you choose to make changes on your own, the following guidelines may be helpful:
Readings at 2-3 hours post-meal give a hint as to how the I:C ratios are working:
- If there is a pattern of low blood glucose 2-3 hours after a given meal, consider decreasing the insulin given for that meal by increasing the “C” in the I:C ratio for that meal (for example, change it from 1U insulin: 10 grams of carbs to 1 unit of insulin for 12 grams of carbs)
- If there is a pattern of high blood glucose 2-3 hours after a given meal, consider increasing the insulin given for that meal by decreasing the “C” in the I:C ratio for that meal (for example, change it from 1U insulin: 10 grams of carbs to 1 unit of insulin for 8 grams of carbs)
- However: If your child’s blood glucose is in-range 2 hours after a meal, and the bolus insulin continues to work for another 1-3 hours (as is typical of insulin action for rapid-acting insulin), there’s a high probability of a low by 3-4 hours post-meal. In this case, you may choose to assess the effect of the current I:C ratio, and balance this against the likelihood of a low.
Tip from the Trenches
This issue (enough insulin to bring BG in target after 2 hours is too much by 3-4 hours) has been a bone of contention for our family…
For example, if we choose a stronger I:C ratio for breakfast, my son’s BG will be in target by snack time at school, which is a good thing. But if he misses that morning snack (such as on the weekends, when the daily routine changes), we are almost guaranteed a low. If, however, we choose a weaker I:C ratio for breakfast, thereby avoiding a low when the insulin is all “used up” at 4 hours, he is likely to be high at school snack time (and then the snack drives his BG through the roof, which takes several hours to come back into target after school). What we have settled on is: a stronger I:C ratio for breakfast on school days, balanced out with a much weaker ratio for snack time (so the end result by lunch is “just enough” insulin overall); on non-school days we manually change the breakfast ratio to be exactly what’s needed for the 3 hours until lunch, so that we do not feel imprisoned by the need to have a snack at 2.5 hours post-breakfast to avoid a low. Another alternative is to leave the breakfast I:C ratio the same every day, and make sure your child has a snack at 2-3 hours after breakfast – the only caution is that you have to be able to ensure the snack won’t be missed, or your child is highly likely to experience a low. ~Michelle
Readings more than 3-4 hours post-meal give a hint as to how the basal rates are working:
- If there is a pattern of low blood glucose 3-4 hours after a given meal, consider decreasing the basal rate for that time period. (For example, change it from 0.200U per hour to 0.150U per hour)
- If there is a pattern of high blood glucose 3 hours after a given meal, consider increasing the basal rate for that time period. (For example, change it from 0.200U per hour to 0.250U per hour)
- Assess the effects of the changes made to pump settings. Are blood glucose readings now in the target range? Moving in the desired direction? Do additional changes need to be made?
Other Notes and Tips about Pump Record Reviews:
- Before adjusting insulin, consider the other factors which may affect blood glucose, such as: exercise, food, less than 2 hours between finishing the meal/snack and checking blood glucose, falsified results, inaccurate readings due to not washing hands, etc.
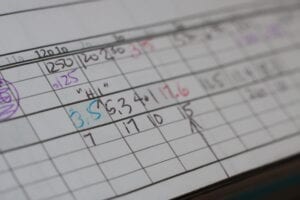
- We have found that a pattern of highs or lows “jumps out” at us if we use a colour coded system in the log book: when we write in a high reading, we use red ink; low readings are logged in blue; target readings are written in black. Rather than keeping 3 pens hanging around, consider buying a pen with 4 colours in one barrel (Bic makes one). Or you could try using pink and blue highlighters to draw attention to high and low readings. Feel free to use whatever system works for you and your family.
- If blood glucose readings do not end up in the target range after following the above steps 2 or 3 times, consult with your diabetes health care team.
Be Aware of Night-time Lows:
- Your review of the log book may not directly show night-time lows. However, high morning readings may, in fact, be an indicator of undetected overnight lows: your child may drop low in the middle of the night, causing the liver to release a large amount of stored glucose to treat the low, resulting in a high morning reading.
- If breakfast/waking blood glucose readings are above 14.0 mmol/L, it is wise to first rule out night-time lows. To do this, set your alarm and check blood glucose at 3 a.m.* for two nights.
- If the blood sugar is low, you may choose to decrease the overnight basal rates.
- If blood glucose highs are not due to a low followed by a rebound , your child may need more insulin overnight. In this case, you may choose to increase the overnight basal rates.
Next Steps in Adjusting Insulin:
The above information was significantly modified with permission from The Alberta Children’s Hospital Diabetes Clinic information handouts.
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE