Time In Range: Strategies to Increase Time Spent in Your Target Glucose Range
Here we offer effective and practical tips for CGM-wearers so you can reduce the swings and spend more time in your target glucose range. Drawing on the knowledge of diabetes experts and personal experience with Type 1 Diabetes (T1D), and summarized from presentations1,2 at the 2021 Diabetes Canada Know No Limits with T1D conference, this concise guide will help you balance your glucose so you can spend less time babysitting the dragon, and more time living your life.
In other Waltzing the Dragon articles, we have explored what “Time in Range” means and whether it really matters in managing Type 1 Diabetes. We have also looked at, in practical terms, what numbers count as “In Range,” how to determine how much time your child is spending in this sweet spot, and how much time that experts recommend we spend in, above and below our target glucose range.
Explore this background information:
How Can I Increase Time in Range?
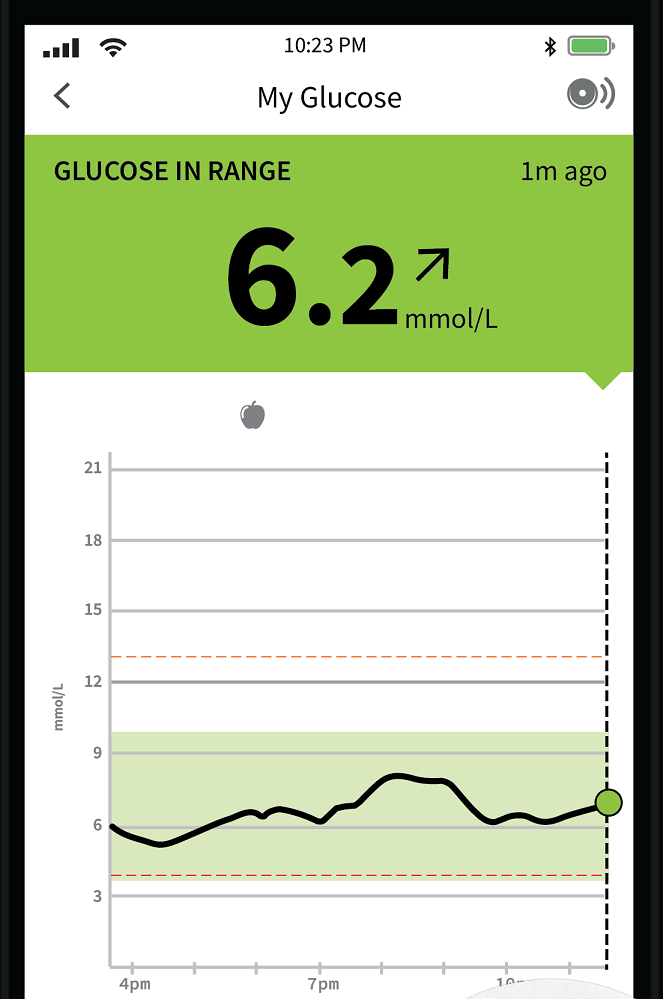
Continuous Glucose Monitoring gives us information about how glucose levels vary that can guide our decisions and actions, so we can be more proactive in how and when we intervene to pre-empt highs and lows.
Here are some strategies that will help you spend more time “in range” (and so less time above range and below range).
1. Look at Lows First
If you are spending more than 15 minutes in a day below 3.0mmol/L, address that first! Not only is low glucose (hypoglycemia) a safety concern, but it also affects the glucose pattern for the rest of the day, so it’s important that your first step toward increasing your Time In Range (TIR) is to resolve any lows.
2. Customize your alerts so that they work for you.
*This tip applies to Dexcom CGM, Medtronic CGM and Libre2. (Libre1 does not include alerts.)
Gabrielle Schmid (RD, CDE, CPT) encourages us to change the alert levels from the general default settings so that you have time to take action before glucose gets too low or too high. Endocrinologist Dr. Ilana Halperin (MD, MSc, FRCPC) agrees, suggesting that we use CGM alerts as a “protective early warning system,” which is especially important during the nighttime. Ms. Schmidt suggests to:

- Set your low alert higher than 3.9, so you have time to take action to prevent a low.
If you receive a low alert, have a small snack. Alternately, if you have no insulin on board, and your glucose isn’t falling too rapidly, you can set a temp basal reduction instead of eating a snack. Note that it takes up to an hour for the results of a temp basal reduction to manifest.
- Set high alerts low enough that you can be proactive in halting the rise. Dr. Halperin agrees that in order to avoid a sustained high, we need to give insulin before glucose gets too high. Consider setting the high alert at approximately 12 mmol/L (especially if your glucose doesn’t often go above that). But since the ideal setting is different for each person with diabetes, so be sure to discuss with your health care provider what would be most appropriate in your individual case.
Tip from the Trenches
In our family, we find that relatively more insulin is needed to correct a very high glucose level, than to correct a moderately high one. (As much as 50 - 100% more insulin is needed to effectively correct a high if our son’s glucose is over 15.0 mmol/L. That’s a lot!) So, if we can catch a rising blood sugar early, then we can correct it sooner with less insulin, and we don’t have to keep chasing the high for hours. -Michelle
In addition, Dr. Halperin suggests that you can guard against alarm fatigue by taking your average glucose level into account when setting alert levels, and then not setting the alert boundaries too tight. For example, if your average glucose currently hovers around 12 mmol/L, then setting alerts at 8 mol/L will result in frequent (and annoying) alarms. Start with smaller changes and then tighten up the high and low alerts in steps, over time.
3. Time Your Insulin
Take your insulin before eating to reduce the frequency and height of post-meal glucose spikes.
4. Look at the Reading AND the Trend
Use your glucose reading and trend arrows to guide your decisions about what to do next. For example, if your child is heading into soccer practice with a 5.0 headed down, they will likely need a snack; but if sensor glucose is 10.0 headed up, a snack is less likely to be needed.
While fingersticks show you one moment in time, sensor-based glucose monitors tell you how you got there (you can look back at last hour or more of glucose data), as well as where you’re headed (trend arrows predict what your glucose will be 15-30 minutes from now), which allows you to make decisions to fit your current situation, so you can positively impact your glucose levels over the next few hours.
Dr. Halperin recommends that her patients look at their CGM trend arrows before dosing insulin for meals, before activity, and before going to sleep at night. She further suggests that we:
- dose mealtime correction insulin based not on where your glucose is right now, but where it will be 15-30 mins from now, both when it’s rising (for example, when glucose is high and rising before supper, for example) and when it’s falling (after exercise, for example).
- be careful about using arrows during Active Insulin time (approximately 4 hours for those who inject their insulin; pumpers will see the current amount of Insulin on Board on the pump screen). If you do decide to deliver a correction dose of insulin the time when you still have Active Insulin remaining in your system, be careful of insulin stacking, which may cause hypoglycemia.
5. Maximize the Mobile
Use glucose data software right on your mobile device (such as the Clarity App, Freestyle Libre 2 app, Guardian™ Connect App) to highlight trends and areas for improvement.
6. Discuss Your Data
Review your glucose data (via Glooko, LibreView, Medtronic Carelink, Dexcom Clarity, or other glucose data software) with your Diabetes Heath Care team. The detailed picture painted by TIR metrics helps them to give you specific strategies to help improve your TIR.
With just an A1C result to work with, Dr. Halperin explains, your Diabetes Educator can tell you that “it’s a little high” or “it’s a little low” but they will not have insight into why. With the TIR metrics, they can see the specific patterns of glucose variability that are behind the A1C average. For example, they can tell if your glucose is spiking consistently after breakfast, or if it’s a bit high throughout the day; they can tell if your glucose levels are fairly stable (low variability overall), or if you are spending some in target with frequent spikes and drops. From there, you can develop a plan to address your specific glucose patterns.
7. Keep Your Eye on the Prize
Between visits with your diabetes educator, track your progress regularly:
- Check your glucose data weekly (in LibreView, Clarity, Carelink, Glooko, or similar) to celebrate and to tweak.
- Get notifications on your mobile device about your glucose data, so that it doesn’t become the “one more thing” that you have to remember to do. The notifications from Dexcom's Clarity, for example, will say things like, “Your Time In Range increased by 3% last week!” This prompts you to reflect on what you did recently that contributed to the Increased TIR. Or the notification may say, “Your TIR decreased by 8% last week,” which is an opportunity to think of one thing you can do in the week ahead to increase your TIR.
The Clarity App also highlights your Best Day, giving you a pat on the back as well as an opportunity to think back on what you did that day that helped manage your glucose. Also, when you achieve your goal (70% TIR, for example) the Clarity App will let you know, which gives the emotional boost that helps keep you going. It’s common to feel beaten down in our efforts to tame the diabetes dragon, tempting to focus on the times that things went off the rails; Best Day shifts our thinking to celebrating the positives!
References:
Understanding Alerts and Time in Range in Real Life, presentation by Gabrielle Schmid (RD, CDE, CPT) at Diabetes Canada’s Know No Limits with T1D conference, Oct 2, 2021 https://nolimitsconference.ca/
Gabrielle is a Registered Dietician (RD), Certified Diabetes Educator (CDE), and Certified Pump Trainer (CPT). She has also lived with diabetes since she was 9 years old.
Tips for Reducing Glucose Variability and Improving Time in Range, presentation by Dr. Ilana Halperin (MD, MSc. FRCPC) at Diabetes Canada’s Know No Limits with T1D conference, Oct 2, 2021 https://nolimitsconference.ca/
Dr. Halperin is an endocrinologist with a special interest in managing diabetes in teens/young adults and during pregnancy, as well as in integrating technology into health care.
SHARE THIS ARTICLE