The Insulin Program We Choose
Is sometimes dictated by circumstance (such as the lack of diabetes support that too many students across Canada face at school), which may push us toward certain types of insulin and insulin delivery methods. But are we aware of what else is available and the pros and cons of each? Find out more about the similarities and differences between the three common insulin programs - Conventional, MDI, and Pump - as well as the pros and cons of each.
Injected Insulin
If your child receives insulin via injections, she will likely take two types of insulin:
- Rapid-acting (to cover food and corrections for high blood glucose), AND
- Either:
-
- Intermediate-acting (as in a Conventional injection program), OR
- Long-Acting (acts as a background insulin, to cover basic metabolic needs: as in a Multiple Daily Injection program)
Pumped Insulin
If your child receives insulin via an insulin pump, she will take only one kind of insulin:
- Rapid-acting
Common Insulin Programs:
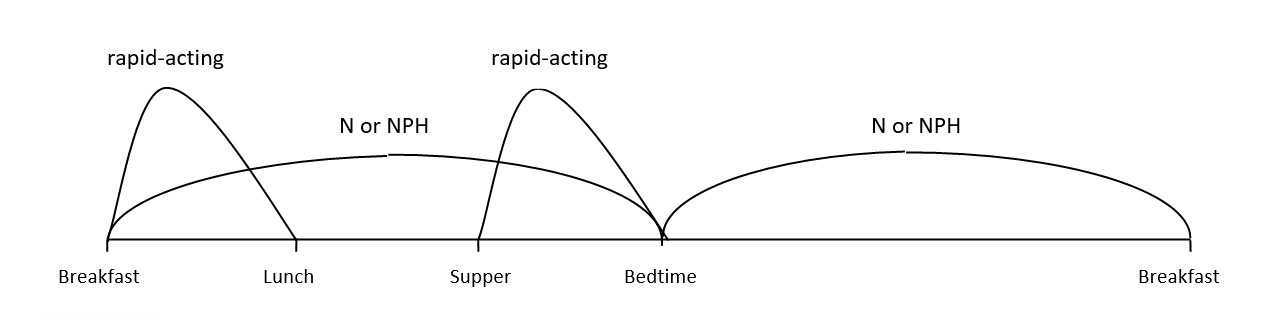
1. Conventional Insulin program
If your child is on a Conventional Insulin Program, she will likely take three injections, which include: an Intermediate-acting Insulin (N/NPH) to act as background insulin as well as to cover lunch and afternoon snacks, PLUS rapid-acting insulin to cover breakfast and supper.
Pros of a Conventional Program (vs. MDI):
- Minimizes the number of injections given (The morning N/NPH covers lunch and afternoon snack) – this is a BIG plus for children who are very resistant to taking their injections.
- Useful (even necessary in some cases) if your child is in school and is not yet self-administering injections (you don’t need to be there at lunch and afternoon snack to administer insulin).
- Useful if your older child or teen does not want to take the time to administer an injection for lunch.
- N/NPH is less expensive than some more recently-developed types of insulin.
- N/NPH can be mixed with other types of insulin (eliminating the need for separate injections when the doses occur at the same time).
Cons of a Conventional Program (vs. MDI):
- Little flexibility in terms of WHEN your child eats: you have to “feed the insulin” (N/NPH) when it peaks (i.e. your child has to eat 6-12 hours after N (NPH) is administered, to match the insulin active at that time); this may be especially difficult with infants or toddlers who may not eat when you want them to; it is also particularly troublesome to “feed the insulin” for the overnight peak (if your child is experiencing overnight lows, you will need to get up in the middle of the night to correct or prevent lows).
Tips from the Trenches
I had a terrible time with my son going low in the middle of the night when he was on N (NPH). I ended up having to give him raw cornstarch mixed in yogurt at bedtime to help with middle-of-the-night lows (because it’s digested at the same time the insulin is peaking).
~ Danielle
- Little flexibility in terms of the AMOUNT your child eats (i.e. you have to feed your child the same amount of carbs everyday at lunch when the insulin is peaking, and the meal should include protein and fat in addition to carbs, in order to slow down digestion of the meal); making and sticking to a meal-plan is a must. If your child is particularly hungry on a given day and she wants to eat more, or if there’s a special treat, like cupcakes at a classroom birthday party, she either needs an extra injection of rapid-acting insulin, or the extra carbs need to be subtracted from her meal allowance. Conversely, if your child is not very hungry on a given day, she still has to eat or drink the predetermined amount of carbs to prevent low blood glucose.
- If your child is growing and therefore eating more overall or if her appetite has decreased, you need to contact your diabetes health care team to adjust N(NPH) dosage (and this dosage change will affect the amount of insulin across the whole insulin-action time (not just at the targeted meal).
- The timing of the peak is unpredictable and is affected by factors such as temperature, injection technique, and mixing technique. This means you don’t know exactly when N(NPH) is going to peak (6-12 hours is a wide range).
Tips from the Trenches
When my son was on NPH, I felt like we had a stalker. We were consumed with the threat of an unexpected low.
~Danielle
- The duration of the insulin action can be unpredictable. N (NPH) can last 12-22 hours; it may last longer than expected, creating a risk of low blood glucose.
- You need to give the intermediate-acting insulin at the same time every day, twice a day. This makes sleeping in or changing morning routine very difficult because a delay affects all other insulin for the day.
It is because of these drawbacks that NPH has been given the apt nickname "Not Particularly Helpful."
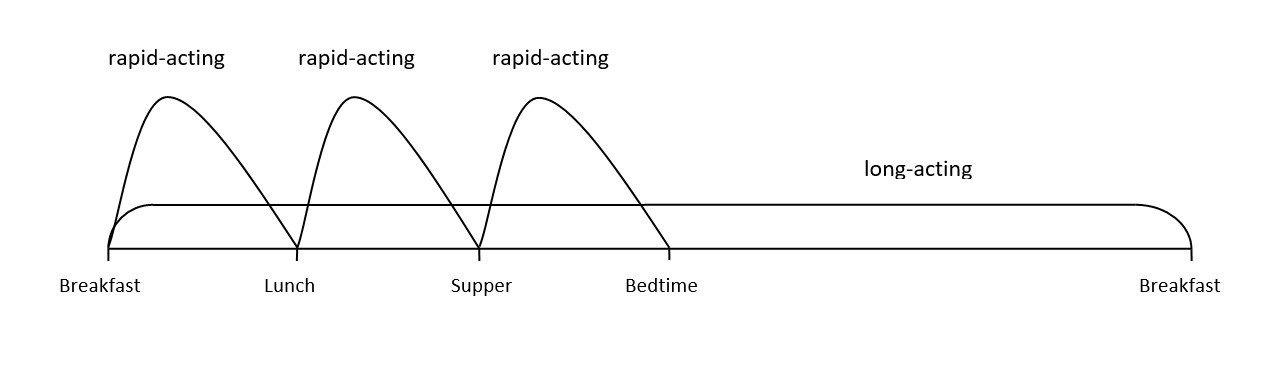
2. Basal-Bolus with Multiple Daily Injections (MDI)
A Basal-Bolus Program with MDI uses a background “peakless” long-acting insulin (such as Lantus® or Levemir®) as basal insulin, plus rapid-acting insulin (such as Humalog®, NovoRapid®, Apidra® or Fiasp®) for all meals (bolus). As the name states, this results in multiple injections each day, as each meal or snack needs to be covered by an injection of rapid-acting insulin.
Pros of a Basal-Bolus/MDI Program:
- More flexibility in terms of the amount your child eats, particularly at lunch (the most restrictive meal under a conventional insulin program). That is, your child is free to eat a huge lunch one day, and a very small lunch the next day.
- More flexibility in terms of when your child eats, which is a big plus for infants and toddlers, who may eat when, what and how much they feel like eating.
- Some people find that the insulin action is more predictable for long-acting (vs. intermediate-acting) insulin.
- Lantus® is usually given only once per day (although for individuals who experience an insulin duration of less than 24 hours, a second dose may be advised by your child’s doctor).
- Lantus® is not affected by injection site, temperature, or injection technique, and does not have to be reconstituted before each injection as cloudy insulin does.
Cons of a Basal-Bolus/MDI program:
- Since there is no sharp peak in the insulin action, Lantus® will not cover food; a separate injection must be given for carbohydrates eaten.
- Lantus® should not be mixed with other insulin. This means your child will have to have a separate injection.
- Frequent injections (may be as high as 8-10/day) means this program may be more appropriate for children who are home for mealtimes (toddlers, home-schooled) and those who can give themselves their insulin. If your child is away at school during the day and does not administer his or her own insulin, this program may require you to go to school at lunch each day to give them their insulin. Also, if your child has issues with injections, this program may create more stress than a conventional insulin program.
Tips from the Trenches
If resistance to injections is a critical issue for your family, please consider the alternatives, tips, and tools outlined under Coping and Family Life, such as Managing the Pain and Fear of Pokes and Tests
Also, Insulflon™ or iPort™ (a flexible cannula that provides a “port” into which you inject insulin, rather than injecting directly into the skin), can greatly reduce the discomfort and hassle of repeated injections.
- Compared to an insulin pump program, you cannot adjust the basal rate for variations in insulin needs at different times of the day. For example, young children often have greater need for insulin a few hours after bedtime to meet their metabolic needs at that time (when growth hormone is released), but if you dose for this time of high need, this may lead to lows later in the night when the insulin need drops. This puts you in a position of having to “feed the insulin” in the middle of the night. Conversely, if you dose to avoid the lows, there may not be enough insulin when the need is high, resulting in a high blood glucose a few hours after bedtime.
- Although the insulin action is thought to be relatively constant, some people report variations in insulin action, which may lead to highs and lows. (Of course, these blood glucose variations are to be expected with any diabetes management program – that’s just part of the diabetes dragon!)
- Some people report that Lantus® “stings” on injection.
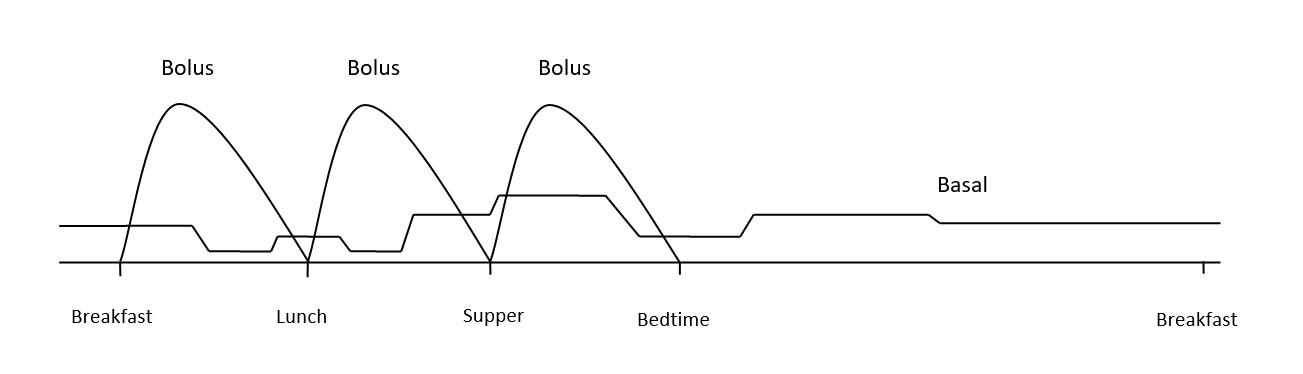
3. Insulin Pump Program
aka Continuous Subcutaneous Insulin Infusion (CSII)
An insulin pump infuses under the skin tiny amounts of rapid-acting insulin (such as Humalog®, NovoRapid®, or Apidra® – Fiasp® is not yet approved in Canada for use in pumps) every few minutes as basal insulin, PLUS delivers a bolus of rapid-acting insulin to cover each meal and snack.
Pros of an Insulin Pump Program:
- Fewer ”pokes”: One “poke” when inserting an infusion set replaces two or more days of injections (a big plus for children who are very resistant to needles); you do not need to give an extra injection for carbs or correction – you simply “dial in” the insulin dose on the pump.
Tips from the Trenches
This is a great plus for parties or other treat times, when my son can run around being a kid, and I can periodically dial in more insulin from his meter remote as he eats more, without having to interrupt his play or make a big deal about it. I still have to count carbs for everything he eats and match the insulin to it, but the delivery has much less fuss involved.
~Michelle
- Basal rates can be customized and individualized, so fluctuating blood glucose patterns can more easily be matched. Not having to give the insulin at a certain time allows for sleeping in.
- You don’t have to “feed the insulin”: a pump can be programmed to give less insulin when insulin needs are predicted to be lower (ex. overnight, or during exercise), as well as to mediate a low-ish blood glucose.
Tips from the Trenches
When our then 3-year-old son was in the 5’s during the night, often we would bring him up a bit by turning the pump down or off, allowing his blood glucose to rise a bit. Before he wore a pump, we would have given him milk in the middle of the night under these conditions. For a true low, however, fast-acting carbohydrate is still the safe choice.
~Michelle
- It’s a portable system. You do not have to remember to bring syringes and insulin every time you go anywhere; your insulin pump is always with you.
- More accurate dosing, in smaller increments: a pump can deliver a bolus of 0.05U (the best we could do with a syringe was 0.5U) and basal insulin can be administered in increments as small as 0.025U. This goes a LONG way towards reducing the blood glucose rollercoaster.
Tips from the Trenches
For example, I give my son a correction dose of 0.30U for a given elevated blood glucose now, but the correction for the same elevated BG on injections would have been 0.50U, according to our sliding scale. So back then he was getting more than he needed (because that was the least I could draw into a syringe), possibly going low later, then high again later because of the low treatment. On a pump, his insulin needs are more precisely matched.
~Michelle
- Physical Accessibility: The pump can be hidden under clothes and easily accessed when needed. Unlike syringes, you don’t have to expose skin to give insulin.
Tips from the Trenches
I remember many times having to take off layers of winter wear from my son just to be able to give insulin (ex. in the car headed out for a day of skiing).
~Danielle
- Simplifies insulin dosing calculations, as all the rates and ratios are programmed into the pump – you only need to input the carbs being consumed and the pre-meal blood glucose, and the pump calculates the insulin dose for you (including any correction for high blood glucose).
- Insulin Pumps use only rapid-acting insulin; you do not have to deal with two separate types of insulin.
- Less insulin stacking (assuming Duration of Insulin Action is programmed correctly for “Insulin On Board” function to make accurate calculations).
- Greater ease and flexibility with regards to exercise (can easily adjust background insulin. just prior to or just after exercise)
- Ease of accessing and analyzing data, as well as sharing data with health care team members.
Tips from the Trenches
My son is able to grab his pump at the end of the day and see, in the bolus history, what insulin has been delivered and when. This comes in handy if he cannot remember if he bolused or not.
~Danielle
Cons of an Insulin Pump Program:
- At times it’s a lot of work, at least initially – many parents we’ve spoken to say that they work harder now that their child is on a pump than they did when she was using injections. To get target numbers you need to constantly analyze and adjust.
- A pump is not the magic solution many envision it to be. It is limited by the brain running it; if it is not programmed correctly, it will not improve blood glucose control.
- When you inject insulin, you know that the insulin is getting in; on a pump, however, if you have delivery problems with the infusion site (bent cannula, scar tissue, poor absorption for any reason), your child may not be getting the insulin that you expect she is getting, which can lead to very high blood glucose.
- There is a greater risk of DKA (diabetic ketoacidosis, life-threatening high blood glucose with ketones) as there’s no long-acting insulin working. This may create a greater need to check your child’s blood glucose during the night.
Tips from the Trenches
I’m not sure whether or not this is a reality of instability or an illusion. But I do know that my husband and I rarely checked our son during the night before he wore a pump – we had checked a few times and detected no problems – now we check at least once, most nights. It’s possible, though, that this need existed before and we just weren’t aware of it.
~Michelle
- Financial Expense: The initial cost is high, as are the ongoing monthly costs for supplies. (Although, if you have an extended health plan, a portion of your pump and supplies may be covered.)
- The pump is worn 24-7, which may feel like a constant physical and emotional burden.
Tips from the Trenches
When my son takes off his pump for short periods he often breathes a sigh of relief and says, “Ahhh… life without diabetes!”
~Danielle
- Although discrete, a pump is a visible sign that your child is “different”, which may be an issue for teens especially.
- A pump does not reduce finger pokes for blood glucose monitoring, as some may expect (and may, in fact, increase the need for monitoring).
- If you go on a pump too soon after diagnosis, before learning the fundamentals of insulin adjustment (i.e. how much insulin to give for how many carbs, and how to correct effectively), you may be ill-equipped to do these calculations if needed (because you’re too used to letting the pump think for you).
References
The above information was based upon, but significantly modified (with permission) from The Alberta Children’s Hospital Diabetes Clinic information handouts.
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE